- Life
Published: | By: Ute Schönfelder
Source article
Whether you have a sports injury, repetitive strain injury or pain in the knee, cortisone preparations are often used to treat acute inflammations. Chronic inflammatory diseases such as asthma, diabetes and chronic inflammatory bowel diseases are also treated with drugs containing cortisone or derived drugs. This is because these drugs usually have a rapid anti-inflammatory effect. However, there are also drawbacks: their therapeutic efficacy is often limited in time, as they work very well at the beginning but their beneficial effects decrease over the course of treatment. In addition, there can be serious side effects, including osteoporosis, increased susceptibility to infections, stomach ulcers and metabolic disorders.
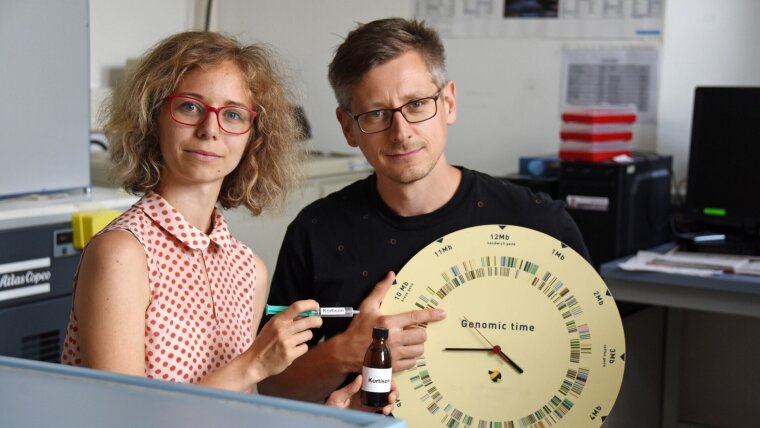
“When using these preparations, it’s therefore important to limit and optimise their use,” says Prof. Oliver Werz, Professor for Pharmaceutical/Medicinal Chemistry at the University of Jena. But when is the optimum treatment window and when is the use of cortisone preparations contraindicated? Until now, there has not been any clear answer to this question. In a recent study, Prof. Oliver Werz and Dr Markus Werner of the Institute of Pharmacy, together with other researchers from the University of Jena, Jena University Hospital and Harvard Medical School (USA), have now clarified an important biochemical mechanism explaining how cortisone preparations mediate inflammation-resolving effects in human immune cells, thus paving the way for an optimised use of these drugs. The researchers present their results in today’s issue of the renowned scientific journal “PNAS” (DOI: 10.1073/pnas.2302070120).
Cortisone influences enzymes involved in the formation of inflammation-resolving messenger substances
In the course of an inflammatory reaction, pro-inflammatory immune cells appear first, including M1 macrophages. They produce pro-inflammatory messenger substances (prostaglandins and leukotrienes), which trigger the typical symptoms, such as fever and pain. After a few days, the second phase follows, in which the inflammation subsides. At that point, macrophages of the “M2” type are increasingly active, which produce inflammation-resolving messenger substances (i.e., resolvins). “In studies on cell cultures, we were able to show that cortisone regulates the activity of certain enzyme genes in the immune cells, which influence the inflammatory process,” explains Markus Werner. In this way, cortisone induces the formation of inflammation-resolving resolvins in M1 macrophages, which appear early, but significantly impairs this function in the M2 macrophages, which appear later.
This effect is regulated by the 15-lipoxygenase enzymes, which occur in two forms in immune cells: 15-lipoxygenase-1 and 15-lipoxygenase-2. “We found that cortisone upregulates 15-lipoxygenase-2 in pro-inflammatory M1 macrophages of the early inflammatory phase. This enzyme catalyses the formation of resolvins, thereby stopping and resolving inflammatory processes, which is partly responsible for the positive effects of cortisone,” says Werner. At the same time, the experiments also showed that cortisone suppresses this resolvin formation in inflammation-resolving M2 macrophages, which is important for healing, by virtually “switching off” 15-lipoxygenase-1. “This explains why the use of cortisone in the later phase of inflammatory diseases no longer leads to symptom relief, and can even be counterproductive and inhibit regeneration processes,” adds Oliver Werz.
From bench to bedside
After the researchers had deciphered the mechanisms at the gene regulation level, they proved these effects in further studies on immune cells from patient samples. They included patients at Jena University Hospital with chronic inflammatory diseases, such as Crohn’s disease and ulcerative colitis, as well as those with severe acute inflammation caused by COVID-19, who were treated with cortisone preparations. Blood was taken from these patients before and after the administration of the medication and examined with regard to the inflammation parameters and enzyme activities. “As in the experiments on cell cultures, we were able to detect a clear upregulation of 15-lipoxygenase-2 in the patient groups treated with cortisone,” notes Dr Benjamin Giszas, a doctor at the Clinic for Internal Medicine IV. Giszas supervised the studies as part of his Clinician Scientist project, funded by the German Research Foundation (DFG).
According to the researchers, their results imply that treatment of inflammatory diseases could be improved by a time-limited use of cortisone and by new 15-Lipoxygenase-based therapy principles, with fewer cortisone-related side effects.
Original publication: Rao Z, Brunner E, Giszas B et al. Glucocorticoids regulate lipid mediator networks by reciprocal modulation of 15-lipoxygenase isoforms affecting inflammation resolution. PNAS 2023, https://doi.org/10.1073/pnas.2302070120External link